When Anton Nikiforov started working in plasma technology, he had no idea he would end up building systems that could revolutionise infection control in hospitals. It all started in the textile sector, where the adhesiveness of the material is critical to the success of the dyeing process. “With the use of plasma technology, you can modify materials in order to enhance the adhesion for any dye,” explains Nikiforov, who is now a postdoctoral researcher at the University of Ghent’s Department of Applied Physics. A relatively simple use of plasma technology, it can be scaled up to industrial applications quickly and easily. Ultimately, Nikiforov and his colleagues were helping their industry partners manufacture hundreds of metres of highly adhesive material per second. He says it was a natural shift into finding more sophisticated uses for the technology. “I wanted to help produce coatings that could be used in everyday life to protect people from disease,” he recalls.
Just as plasma technology can modify the surface of a textile-based material to allow dye to stick to it more strongly, it can manipulate how different items in healthcare settings – from masks and surgical instruments to often-touched surfaces – react to bacteria. “Antibiotics are not our future. Today we are using antibiotics that are second or even third generation and bacteria are adapting to that very fast; it’s more and more difficult to develop smart antibiotics that can keep up,” Nikiforov says. “Plasma technology takes a different approach, using direct interaction between the microorganisms and surfaces to either kill bacteria immediately or prevent it from sticking to surfaces. This is definitely something hospitals will need in the future. And not only hospitals, but all of us.”
A cheaper, greener, more flexible method
The development of antimicrobial materials has increased significantly in recent years, due to the increase in antimicrobial resistance and hospital-acquired infections. More than 2.8 million antibiotic-resistant infections occur in the US each year and more than 35,000 people die as a result. Meanwhile a 2021 study by researchers with the Centres for Disease Control and Prevention (CDC) showed that, after years of decline, US hospitals saw significant increases in healthcare-associated infections (HAIs) in 2020, driven largely by the Covid-19 pandemic.
The technology being developed by Nikiforov and his colleagues at the University of Ghent, in collaboration with research groups in the Czech Republic, Italy, Slovenia and Romania, differs from existing methods used to create biocidal materials in two important ways. “In general, these types of materials are produced by mixing a number of chemicals with your solvents, so you are using really heavy chemistry. Typically, it’s not a very green process, and it’s slow and expensive,” Nikiforov explains. “In addition, those techniques are typically substrate-dependent, so you can make them for one polymer but not for another.”
Plasma technology, on the other hand, uses a limited number of chemicals in extremely small quantities and can be used for many different types of materials. “With the same technology we use to make coating on polymers, we can move to fibres, metals, glass, any kind of substrates. This is very interesting for the healthcare industry. They can start with one process and easily scale it up or modify it to be applied to another.”
How does it work?
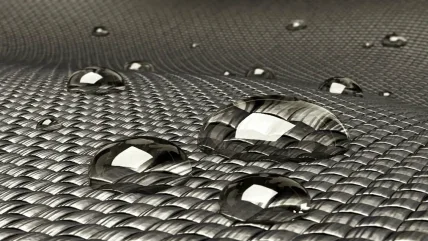
The technology behind plasma-based surface engineering relies on nonequilibrium plasma, or partially ionised gas, that produces chemical reactions to change the properties at the material surface. Nikiforov and his colleagues have developed three different ways to manipulate the make-up of materials to either prevent bacteria from sticking to them (antifouling), or kill it instantly on contact (bactericidal). Anti-fouling materials prevent microorganisms from accumulating on surfaces to form biofilms and other dangerous microbial environments. “A typical example would be coatings based on fluorine-containing functional groups, similar to Teflon, that mean liquids cannot stick to the material,” Nikiforov explains.
The bactericidal system on the other hand destroys microorganisms on contact by puncturing them with microscopic spikes. “Bacteria are basically killed by touching the material,” Nikiforov says. “You make some very tiny nano-scale needles on the surface and when bacteria stick to them, they penetrate the membrane and kill it.”
The last technology, and Nikiforov’s favourite, combines anti-fouling with drug release. “Typically, we use different nanoparticles of copper or silver. When bacteria touches the surface, small quantities are released from the surface and can penetrate and kill bacteria. We are trying to develop this for different materials, including instruments and masks, which are often used in hospitals.”
Performance and toxicity
In the lab at Ghent University, Nikiforov and his colleagues haven’t reached a level of industrial application for their technologies yet, but they are treating up to a few metres squared worth of materials. The next step is to bring in engineers with ideas on how to scale them up. “It is very demanding, not only to understand the physics, but to know how to control it. If you move to industrial level, you need to run it every single day,” Nikiforov explains.
In addition to controlling the performance of the factory line, the team need more help from safety and bioengineering experts. “You can combine single nanoparticles and integrate them in a coating and it will be antibacterial. But that antibacterial coating could also be very toxic,” Nikiforov says. “The point for us is to find not only engineering skills and engineering partners to make machines bigger but also to find people who are very knowledgeable in the interaction of materials with bacteria and cells to be sure that our antibacterial coatings are purely antibacterial and not toxic.”
Even to reach the point the researchers are currently at has required a massive team effort. “You need chemists, people who are working in physics like me, people working on the engineering side, people working on the biological side. For such complicated research, an interdisciplinary team is essential. This has started to be one of the trends that we see: only in cooperation with other partners can this kind of technology be developed.”
Moving the technology to market
Just as Covid-19 has shown that vaccines can be developed, marketed and sold more rapidly than many people thought possible, plasma technology-based masks designed to prevent Covid-19 infection, which work on a similar principle to plasma-based antibacterial surfaces, have already reached pharmacies. “That team worked incredibly hard for the past two years; it was really hard to evolve this to a real application,” Nikiforov says.
However, this will likely be the exception to the rule. “What I see from my experience is that the minimum term is about three to four years to move something to market if you already have a technology,” says Nikiforov. “It’s not only about proving that your technology is operational, but changing mindsets around old-fashioned techniques, and this is not easy.”
A different angle
The technologies developed through the University of Ghent collaboration are just one approach to the wider issues of reducing hospital acquired infections and tackling antibiotic resistance. For Nikiforov, some of the most exciting research being undertaken comes at the problem from a completely different angle. “Instead of making coatings that kill bacteria, they are trying to make some kind of surface which itself can make plasma,” he says.
In essence, it’s a textile, which is coated with a flexible electrodes system. You can switch on the plasma technology at any time, so it will destroy bacteria. “Whatever bacteria they touch will be destroyed. And because it’s a technology based on active species, bacteria have no weapons to protect themselves from this,” Nikiforov explains
He envisages an operating theatre of the future where tools like endoscopes have an integrated plasma lining, which can be activated after surgery to kill bacteria. Tubes for dialysis could be similarly coated. “The techniques used now, like sterilization, are based on heating or on chemicals, which are abrasive to the endoscope itself. But with plasma, you can do the same in a matter of seconds and no bacteria can touch it because they will all be killed,” he says. “I’m really looking forward to the future, to seeing what will be developed in the coming years.”
2.8 Million
The antibiotic-resistant infections that occur in the US each year, more than 35,000 people die as a result.
CDC



